Applying Ethical Principles Within Implementation Research
Authorship: The following blog was written by Shannon King, a MSPH candidate at Johns Hopkins Bloomberg School of Public Health, who has been volunteering with SISN. The information reflects the ethics in implementation put forward in the peer-reviewed literature.
Research ethics for intervention studies in clinical settings are well established. However, research ethics for implementation research (IR) in low-middle income countries (LMIC) has not been as clearly delineated. In our previous blog post “When does implementation research require ethics approval?” we highlighted steps to consider when navigating the ethics review process. Regardless of the need for formal ethics review, all forms of research should adhere to basic human ethics principles. The three ethics principles outlined in the Belmont Report (See Box 1) offers useful guidance when evaluating the ethical implications of your own work.
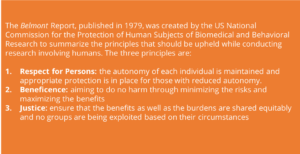
Box 1: What is The Belmont Report?
- Respect for Persons within Implementation Research:
Respect for persons guides researchers to make decisions to protect the autonomy of their participants, and that vulnerable groups with reduced autonomy (e.g. children) receive additional protections. In practice, applying this principle means obtaining informed consent and maintaining each participants’ privacy.
Informed Consent
The Belmont Report outlines three elements of informed consent 1) information 2) comprehension and 3) voluntariness. Thus, researchers must provide participants with adequate information, ensure that the individual understands the potential risk and benefits of their participation and that each participant is voluntarily deciding whether or not to be involved (3). Even if consent is obtained, research subjects maintain the right to abstain from parts of the study, terminate their participation, or revoke their consent at any point throughout the research without penalty.
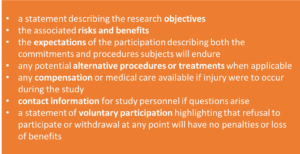
Box 2: What Information Should be Included in a Consent Form?
A well-written consent statement (See Box 2) should provide accurate information presented in language, both in terms of comprehension and dialect, that is understood by study participants (5). The information should be presented in a way that is respectful to traditional beliefs regardless of the differing understanding or beliefs of the science behind the intervention (6).
During the consent process the research team needs to create an environment where the participant knows their consent is voluntary. Researchers should identify and do their best to remove the pressure felt through implicit power dynamics, such as highly trained and skilled researchers working with low resource and low educated subjects, and explicit power dynamics, such as a traditional hierarchy within the community (1, 7). Additionally, if any compensation is being provided, it should be critically assessed to ensure individual’s participation is not induced or exploited.
When research is not considered human subject, there are no legal obligations to acquire written informed consent; however, to maintain the ethical integrity, informing participants of the study aims and processes is good practice.
Participant’s Privacy
Beyond informed consent, Respect for Persons includes protecting the subjects’ right to privacy throughout the entirety of the research process. Only necessary personal identifiers should be collected in a safe and private environment (2). The information should be de-identified and stored in a controlled environment with personal identifiers stored separately. All local privacy laws and regulations should be followed.
- Beneficence within Implementation Research
The principal of Beneficence ensures that research is conducted with the best interests of the participants in mind; thus, researchers aim to minimize the risks and maximize the benefits of their work (4). Within IR this can be challenging to justify as in many cases the risk is at the individual level while the benefits are expected within the greater community (1, 7). In some situations, the groups exposed to the risk are different than the groups experiencing the benefits, which creates a complicated risk-benefit analysis. For example in vaccination implementation trials; those who receive the vaccination are subjected to potential effects of the immunization alongside the reduced risk of disease. For the other group who did not receive the vaccination, they are not at risk of the negative side effects, but they still benefit from a reduced risk of disease transmission due to the herd immunity effect (7). It should be ensured that no group is knowingly being exposed to significant risk for the benefit of another group, however where the threshold of risk sits is extremely contextual. The literature suggests gathering input from community and stakeholder consultations to help assess what is appropriate in the context (8) and that whatever is ultimately decided is clearly explained within the informed consent process.
Equipoise
Within clinical research, one of the key principles of Beneficence is equipoise, which refers to the assumption that within a randomized control trial neither the control or experimental group is receiving an intervention that is knowingly better (9). This ensures that no patient is provided a treatment that is known to provide more benefit (9). The unknown efficacy of the intervention being researched helps justify the risk-benefit balance and upholds the “do no harm” ethical standard.
When IR is based upon already proven efficacious interventions (10) therefore clinical equipoise is no longer relevant. Within experimental IR, contextual equipoise, referring to the researcher’s genuine uncertainty if the intervention will function within a given setting or which implementation strategy is most effective, is the equivalent concept to clinical equipoise (1). If the researcher is able to demonstrate an uncertainty of how the local context influences the implementation, and that the control group is receiving the highest known standard of care, then the research can be justified.
- Justice within Implementation Research
Justice aims to ensure that the benefits and burdens are shared equitably and that no groups are being exploited (4). Ensuring justice in research begins with selecting subjects based on research needs rather than convenience. Inclusion and exclusion criteria should be explicit within the research protocol and followed to ensure equal opportunities to the participants (1, 4). Within IR this has been applied through ensuring appropriate selection of research subjects (4).
In conclusion, the implementation of nutrition programs and the conduct of IR in this context can be associated with unique ethical challenges. Literature describing the specific ethical issues raised by public health interventions in the fields of undernutrition, breastfeeding, vitamin/mineral supplementation and food fortification, food security, food sustainability and food safety is currently sparse (11). It is important that ethics becomes a key consideration in nutrition policy and program development to prevent serious and potentially irreversible ethical problems emerging during implementation and scale up (11). Ethical issues can be complex, as such, each ethical issue needs to be addressed on a case by case basis. Consequently, one should consider all three ethical pillars outlined in the Belmont Report during the design process and uphold them through the conduct of the research to ensure all participants are protected from harm.
References
1.Macklin, R. (2014). Ethical challenges in implementation research. Public Health Ethics, 7(1), 86-93.
2.Protection of Human Subjects, 45 CFR § 46 (2009).
3. Institutional Review Board, 21 CFR § 56 (2015).
4. The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. (1978). The Belmont report: Ethical principles and guidelines for the protection of human subjects of research. Bethesda, Md: The Commission.
5. World Health Organization. (2014). Implementation research toolkit. Geneva; Switzerland. World Health Organization.
6. Lasser, J., Gottlieb, M.C. (2017). Facilitating informed consent: A multicultural perspective. Ethics & behavior, 37(2), 106-107.
7. Gopichandran, V., Luyckx, V.A., Biller-Andorno, N., Fairchild, A., Singh, J., Tran, N., … Vahedi, M. (2016). Developing the ethics of implementation research in health. Implementation Science, 11 (161), 1-13. https://implementationscience.biomedcentral.com/track/pdf/10.1186/s13012-016-0527-y
8. Hyder, A.A., Rattani, A., Krubiner, C., Bachani, A.M., Tran, N.T. (2014). Ethical review of health systems research in low- and middle-income countries: a conceptual exploration. The American Journal of Bioethics 14(2), 28-37.
9. Miller, F.G. (2012). Clinical equipoise and risk-benefit assessment. Clinical trials. 9(5), 621-7.
10. Peters, D.H., Tran, N.T., Adam, T. (2013). Implementation research in health: a practical guide. Geneva, Switzerland; World Health Organization.
11. Hurlimann T, Peña-Rosas JP, Saxena A, Zamora G, Godard B (2017) Ethical issues in the development and implementation of nutrition-related public health policies and interventions: A scoping review PLOS ONE 13(2): e0192356 http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0186897
Have an idea or a comment on any of the issues discussed above? We welcome your feedback – you can comment on this post on our LinkedIn feed or write to us using the email address below.
To learn more about SISN and become a member, please contact us via our website (www.implementnutrition.org) or can email us at implementnutrition@gmail.com.

